From patient to physician-scientist with St. Jude Fellow Bradley Muller, MD
St. Jude Fellow Bradley Muller, MD
When I was 8 years old, going through treatment for T-cell acute lymphoblastic leukemia (T-ALL), I decided I wanted to be a doctor. Even then, I knew I wanted to grow up to help kids with cancer. Back then, in 1998, part of my healing journey was trying to figure out how to make something positive from this entirely traumatic experience, not only for me but also for my family. I became close with my oncologist during treatment and liked the way that they worked with my entire family, their whole staff and me. There and then, I decided that I wanted to be one – a doctor taking care of kids with T-cell ALL and figuring out better therapies for them.
I’m now in my third year of pediatric hematology/oncology fellowship training at St. Jude. I remember the moment I chose St. Jude – I was ending my residency at Johns Hopkins and looking for the right place to take my next career step. In my opinion, no one does translational research better than St. Jude. That’s largely because the labs are directly adjacent to the hospital, allowing a seamless relationship between scientists and clinicians. It was the perfect fit for what I wanted professionally. St. Jude quite literally sets the standard for B-cell ALL (B-ALL) treatments. It’s hard to beat excellent survival in the patients with standard-risk B-ALL. Given those results, it seemed like a promising place to pursue T-ALL treatment research.
But the attraction to clinical practice here extends well beyond the excellence in ALL treatment. All of St. Jude clinical care has a very specific philosophy. Since I first encountered the idea, I have loved the concept of taking care of the entire family through the full time of treatment, just like my pediatric oncologist did for my family. But even with best-in-class clinical practice and family support, St. Jude is a research institution – it’s literally in the name. This gives fellows the opportunity to be both doctors and researchers – it’s an invaluable flexibility for someone just starting their career.
Pursuing translational research in the lab
At St. Jude, you can do the project that suits you. Fellows participate in basic, clinical, and global research – the focus of which is your choice. Of course, I wanted to study pediatric T-ALL and really understand why outcomes have not improved much from when I was treated to come up with new potential treatments. The fellowship program director Hiroto Inaba, MD, PhD, St. Jude Department of Oncology, helped connect me with the right people for my research project. He knows what our personal goals as fellows are – and where on campus the expertise on our interest exists.
When I clarified my plan for the project, which would heavily involve T-cell receptor biology, he introduced me to Paul Thomas, PhD, St. Jude Department of Host-Microbe Interactions, one of the field’s leading experts. Without Inaba, I would not have found Thomas. It’s one of the main reasons I’m here, and why my fellowship has been so successful.
In the Thomas lab my work is focused on gamma-delta T-cell receptor biology in a rare subtype of T-ALL, appropriately termed gamma-delta T-ALL. The cancerous T cells express a gamma-delta T cell receptor but use it in an aberrant way. This is particularly dangerous, as the receptor binds things to cause the T cell to activate and proliferate, a causal link to cancer.
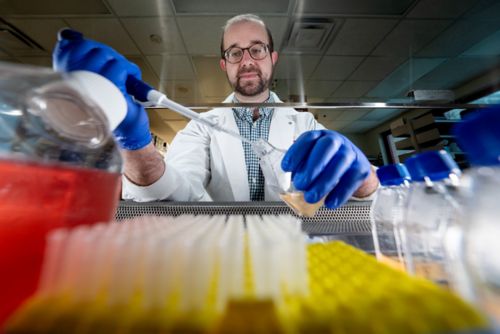
Muller in the cell culture hood manipulating samples.
I’m trying to understand the biology of these receptors to find a better translational therapy. This could be an approach such as generating chimeric antigen receptor (CAR) T cells to destroy those cells with a certain type of receptor. It could also be an approach that used a small molecule inhibitor, or cocktail of them, to intervene in the activation pathways downstream of T-cell receptor activation.
I’m partially motivated to find these new treatment approaches because I received cranial radiation for my cancer, with some significant late effects. I want to make therapies less toxic for these kids. I'd like to prevent radiation use so they don't have to deal with this. Ching-Hon Pui, MD, St. Jude Department of Oncology, designed the modern standard of care protocols that avoid radiation use. I’ve been dealing with these late effects for 20 years now, so I am compelled to follow the standards set by Dr. Pui to find a way to prevent or minimize collateral tissue damage with any novel therapy protocols I develop.
In addition to that main project, I’ve also worked with Inaba on a different clinical research endeavor, looking at T-ALL. We’ve collected data from nearly 200 patients, which I’m analyzing. Inaba brought me onto the project because he knew of my research interest in T-ALL, and thought it fit the type of research I’d like to be engaged in. Instead of causing friction with Thomas, who is technically my principal investigator, he actively wants to know what his lab can learn from this other project. It is this spirit of collaboration and free-flowing information that makes St. Jude such a fantastic place to train.
The combination of scientists and physicians facilitates collaboration and discovery
Speaking of working in the Thomas lab, I must also mention how instrumental the kindness and collaboration of his lab members has been. When I started my fellowship, it had been years since I had performed basic lab research, so my colleagues helped train me on their techniques and assays. The lab is comprised mostly of postdoctoral fellows, staff scientists and graduate students. While they gave (and still give, if I’m being honest) patient and practical guidance on experimentation, they also appreciate my unique perspective and what I can offer the lab, as both a physician and former patient.
Many of my academic colleagues focus on oncology-related projects, but they have not had a clinician regularly looking at their work. So, the perspective I bring in is, "Well, why does this matter?" We can get down into the nitty-gritty details of the biology of these things, but at the end of the day, I want to know why it matters. I often help consult on how to take it to the next step from esoteric data to potential translation. I’ve learned that a physician-scientist can provide valuable insights in this lab environment, especially when combined with the practical realities of the patient experience.
Of course, your research projects and lab relationships only matter if you have time to maintain them. The opposite horror story of being locked in a lab is being on-call for the clinic so much that you never get a chance to do any research. What’s great about St. Jude is that we have true protected time here. I may have the pagers for taking calls every month or month and a half for one night, but that’s a drastic reduction from other programs, with real consequences for my research. I am well-rested and can go to lab and be highly functional in an intellectually challenging environment.
The focus of everyone at St. Jude is improving outcomes for patients. And that only comes from new primary research, which the institution recognizes requires focused time. Everyone, from scientists to clinical staff, has been highly encouraging of my projects, including giving me the time I need to work on them.
Finding my place in the St. Jude fellowship
For me, St. Jude has been a great fit for both my research and pediatric hematology-oncology specialization. I’ve found my place here, studying a cancer that has been an intimate part of my life since childhood. From my treatment to investigating in the lab, I’ve really come full circle. I also participate as a patient advocate because I think it’s important for a family that has a child newly diagnosed with ALL to see that, "Oh, he got through this. He's done okay for himself." I think that's important for families to see. I’m officially a physician-scientist, practicing family-centered medicine while researching how to better treat the ALL subtype that once threatened my life.
I hope any interested future physician-scientists will seriously consider applying to the same program to set a similar foundation for their careers.






